AKI secondary to UTI
- Get link
- X
- Other Apps
This is an online e-log platform to discuss case scenarios of a patient with their guardian's permission.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including, history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
★ CASE SCENARIO :
•A 58 year old male patient came to casualty with chief complaints of:
- lower abdominal pain: 1 week
-burning micturation:1week
- low back ache after lifting weights
-dribbling / decrease of urine out put:1week
-fever :1 week
- SOB , rest :1week
1. COMPLAINTS AND DURATION:
-week back , after weight lifting
Patient had sudden onset of pain in abdomen
By burning micturation with high fever : grade associated with chills and rigor
Decrease urine output associated with SOB (grade -4)
With no H/O chest pain, palpitations, pedal oedema, facial puffiness.
2.HISTORY OF PRESENT ILLNESS
-H/O NSAISD use present, Regularly for body pains and headache
-No photo phobic, phonophobia , giddiness nausea, vomiting, tinnitus
- blurring of vision, black outs
3.HISTORY OF PAST ILLNESS
RTA 13 years, trauma to head , CT brain
Shows minimal bleed - used medication for 3 months
K/C/O - HTN: 1 year (not on medication)
N/K/C/O- DM-2 ,TB, epilepsy ,CNA ,CAD
4.TREATMENT HISTORY :
Diabetes-No
Hypertention- No
CAD-NO
Asthma -No
Tuberculosis -No
Antibiotics - No
Hormones-No
Chemo/Radiation -No
Blood Transfusion -NO
Surgeries - No
Other- No
- There is no usage of drugs as now
5.PERSONAL HISTORY :
- Married
- Occupation : mechanic
- Apettite : Lost form 1 week
- A non vegetarian
- Bowels : irregular
- Micturition : abnormal
- No H/O known drug allergies
-Alcohol : regular ( 3times a week)
-Tobacco -No
-Drug use -No
-Betel nut - No
-Betel Leaf (Pan) - No
6. FAMILY HISTORY :
- NAD
PHYSICAL EXAMINATION :
A) GENERAL EXAMINATION
Pallor- NO
lcterus-NO
Cyanosis-No.
Clubbing of fingers/toes- No
Lymphadenopathy-No
Oedema of feet- No
Malnutrition - No
Dehydration -no
- Temperature : Afebrile
- BP : 140/70mmHg
- PR : 88bpm
- SPO2 : 95% at room air
-GRBS:113 mg%
SYSTEMIC EXAMINATION:
B) CVS
- Thrills : No
- Cardiac sounds - S1 , S2 heard
- Cardiac murmurs : No
-IVP increased
C) RS
- Dyspnea : No
- Wheeze : No
- Position of Trachea : central
- Breath Sounds : vesicular
- Adventitious sounds : No
D) ABDOMEN
- Shape of abdomen : Obese
-tenderness present(in supra public pain RIF)
- No palpable mass
- Hernial orrifices : Normal
- No fluids , bruits
- Liver and Spleen are not palpable
- Bowel sounds : yes
- Genitals : Normal
E) CNS
- patient is conscious
- speech is normal
- No focal neurological defect is seen
-Glasgow scale :15/15
★ REFLEXES
- Plantars : flexor
★ CEREBRAL SIGNS :
- Finger - nose and Knee - Heel are in coordination
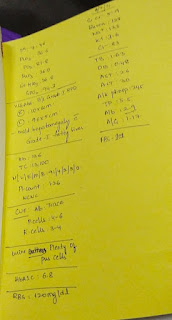
SEROLOGICAL INVESTIGATIONS: ON 6/07/21
pH : 7.46
PCo2 : 36.6
PO2 : 81.8
HCO3 : 26.0
St.HCO3 : 26.8
SPO2 : 94.3
________
USG Abd : B/L Grade -1 RPD
Rigth:10×6cm
left:9.6×5cm
-mild hepatomegaly with Grade-1 fatty liver
________
Hb-13.6
TLC-13,100
N-91
L-04
E-02
M-03
B-00
PLT(plateletcount)-1.26
________
Clinical Urine Examination:
Pus cells-4 to 6
Epithelial cells-3 to 4
Alb: Trace
________
Urine: plenty of pus cells
________
HbA1C : 6.8
________
RBS : 120mg/dl
________
Serum creatinine: 5.9 mg/ dl
Blood urea: 128 mg/ dl
Sodium : 133 mEq/L
potassium : 3.6 mEq/L
chloride : 53 mEq/L
_________
Liver Function Test:
TB -1.63
DB -0.48
AST -26
ALT -30
Alkaline Phosphate-245
TP:5.5
Alb-2.9
A/G-1.17
__________
FBS-101
★ INVESTIGATIONS :
ON- 6/7/21
-HbA1c :6.8%
-Random blood sugar :120mg/dl
-Serum electrolytes:
Na: 133mEq/L
K: 3.6mEq/L
Cl:83mEq/L
-Blood urea:128mg/dl
-serum creatinine :5.9mg/dl
Complete urine examination (CUE):
Colour: Pale Yellow
Appearance: Clear
Reaction: Acidic
Specific gravity: 1.010
Albumin:Trace
Sugar:Nil
Bile satls:Nil
Bile pigments :Nil
Pus cells : 4 to 6
Epithelial cells: 3 to 4
RBCs:Nil
Crystals :Nil
Casts: Nil
Amorphous deposits :absent
Others: nil
ON - 7/7/21
-BACTERIAL CULTURE AND SENSITIVITY REPORT:
Nature of specimen: Urine
- plenty of pus cells (>10/HPF) seen
-culture report: Polymicrobial flora
HbA1c : 6.5%
FBS : 101mg/dl
PLBS : 147 mg/dl
* Total count – 15,400cell/cumm
* Neutrophils - 80%
* Lymphocytes - 10%
* Eosinophils - 04%
* Monocytes - 06%
* Basophils -00%
* PCV – 33.6VOl%
* MCV – 85.9fl
* MCH - 29.2 pg
* MCHC – 33.9%
* RDW-CV – 13.5%
* RDW-SD – 42.9fl
* RBC COUNT – 3.91 millions/cumm
* Platelet count – 4.3 lakhs /cumm
* Smear
- RBC – NORMOCYTIC NORMOCROMIC
- WBC - Leukocytosis
- Platelets - Adequate
- Hemoparasites - Not seen
- impression - NORMOCYTIC NORMOCROMIC with Leukocytosis
★ PROVISIONAL DIAGNOSIS :
- AKI 2° to UTI, associated with Denovo - DM -2
-With ? Right HEART FAILURE,
-With K/C/O - HTN ( Not on Rx)
TREATMENT:
1)IVF : -RL @ UO+ 30ml/hr
-NS
2)SALT RESTRICTION < 2.4gm/day
3)INJ TAZAR 4.5gm IV/TID
|
2.25gm IV/ TID
4)INJ PANTOP 40mg IV/OD
5)INJ THIAMINE 1AMP IN 100ml NS IV/TID
6)INJ HAI S/C ACC TO SLIDING SCALE
8AM - 2PM - 8PM
7)SYP LACTULOSE 15ml PO/TID [ To maintain stools less than or equal to 2]
8) GRBS - 6th Hourly
9) BP/PR/TEMP - 4th Hourly
10) I/O - CHARTING
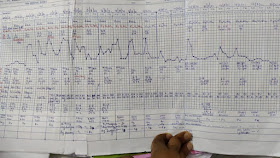
ON 10/7/21 :
- Get link
- X
- Other Apps