This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE
80 year old male came to the opd on 15/6/2021 with chief complaints of
Burning micturition since 4 months
Increase in frequency of urination since 4 months
Thin streaming of urine since 3 months
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 months back, then developed fever with chills which is high grade, continuous and associated with burning micturition and increased frequency of urination.Fever was relieved on medication but burning micturition and increased frequency of urination was persistent.
He complaints of lower backache when there is increased frequency of urination.
Presently there is no complaints of fever, cold, cough.
No hesitancy of urine
No complaints of abdominal pain, pedal edema, facial puffiness.
PAST HISTORY
He is not a known case of Hypertension, Diabetes mellitus, Asthma, CAD, TB
No surgeries in the past.
PERSONAL HISTORY
Diet- Mixed
Appetite- normal
Bowel and bladder movements - regular
Sleep - adequate
No allergies
Addictions:occasional toddy drinker
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
The patient is examined with informed consent.
Patient is conscious, coherent and cooperative ,is well oriented to time, place and person.
He is moderately built and nourished
Pallor : absent
Icterus : absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Pulse:82 BPM
Respiratory rate :18 cycles/min
BP : 110/60mm HGHG
SYSTEMIC EXAMINATION
CVS:
S1 and S2 heart sounds heard.
No murmurs heard.
Respiratory system:
Bilateral air entry
Vesicular breath sound
CNS
Intact oriented to time, place and person
Abdomen
Soft and non-tender.
Bowel sounds were heard.
No organomegaly
INVESTIGATIONS
CBP
CUE
Serum creatinine
RBS
Ultrasound abdomen
Blood culture
Urine culture
PROVISIONAL DIAGNOSIS
Urinary tract infection with grade 2 prostatomegaly
TREATMENT REGIMEN
TAB NITROFURONTOIN
TAB UROMAX
PLENTY OF ORAL FLUIDS
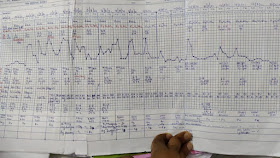
TEMPERATURE CHARTING EVERY 4TH HOURLY









Comments
Post a Comment