Final Exam Long case
Long case
H no 1601006033
This is an E log book to discuss our patient de identified health data shared after taking their consent.
A 51 year old male patient resident of miryalaguda occuption by farmer came to the opd with the chief complaints of
1.Fever since 10 days
2.Cough with sputum since 10 days
3.Shortness of breath since 7 days
History of presenting illness:
Patient was apparently asymptomatic 10 days back, then he developed fever with chills and rigors which was insidious in onset with diurnal variation more at night which was relived on medication.He then developed expectorate cough which was insidious in onset, gradually progressed more during the nights.It aggrevated during exposure to colder climates.The sputum was scanty and yellow which was non foul smelling. Cough was associated with chest pain which was non radiating and aggrevated on lying down and relieved on sitting upright.He later developed Dyspnoea which was insidious in onset ,gradually progressive to an extent that intereferes his daily activities (indicating MMRC grade 4) and eventually progressed to orthopnea.
No history of wheeze
Past history:
No history of Asthma, Tuberculosis, Hypertension, Diabetes Mellitus, Seizures
Known case of COPD (6 years recurrent attacks of exacerbation twice a year are seen)
Family history:
Not relevant
Personal history:
Sleep :Disturbed due to SOB
Bowel and bladder:Regular
Appetite: Normal
Diet: mixed
Smoking :Since 40 years(10 beedis per day)
(Smoking index:5×40=200)
Alcoholic:Since 40 years
General Examination:
Patient is conscious, coherent, co operative.
Undernourished
Vitals:
Pulse:82 bpm(regular, normal in volume)
Blood pressure:100/70 mmhg
Respiratory rate: 29 cpm
On physical examination
Pallor -Absent
Icterus- Absent
Cyanosis- Absent
Clubbing-Absent
Lymphadenopathy-No palpable lymphnodes
Edema - No edema
Systemic examination
Examination of respiratory system
Inspection of upper respiratory tract:
Nostrils are normal
No deviated nasal septum
No nasal polyps
No enlarged tonsils
Posterior pharyngeal wall appears to be normal
Inspection of lower respiratory tract:
Shape and symmetry: elliptical and symmetrical
Spine appears to be in central
Trachea appears to be in Central
Respiratory movements :Decreased on both sides
Breathing pattern was Thoracoabdominal
No visible pulsations
No visibe scars
No visible sinus
Palpation
Spine : central
Trachea: central
Apex beat: palpable on left side 5th intercoastal space
Chest expansion equal on both sides
Dimensions:
Anterior posterior diameter:16.5 cm
Transverse diameter: 23.5 Cm
Chest circumference:73.5
Vocal fremitus :increased on left infraclavicular and mammary region
Percussion
On percussion hyperresonant heard on Left infraclavicular
Left infrascapular
Left mammary.
Auscultation
Tubular breath sounds are heard
Vocal resonance increased in left infraclavicular and left mammary region
Crepitations heard on left infra axillary region
Other systems
Cardiovascular system examination
S1, S2 heard
No murmurs
Apex beat felt on 5th intercoastal space
Gastrointestinal examination
Soft, non tender, no organomegaly, bowel sounds present
Central nervous system examination
No focal deficits seen
Differential Diagnosis
1.Exacerbated COPD
2.Pneumonia
3.Tuberculosis
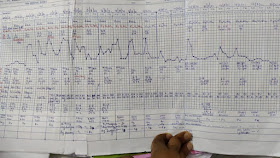
Investigations
Provisional Diagnosis
Consolidation in left apical region
Probably due to exacerbated COPD with infective etiology
Treatment recieved till now















Comments
Post a Comment